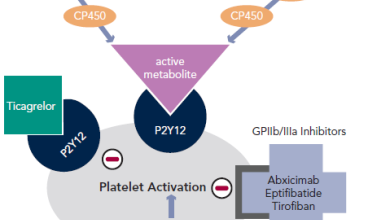
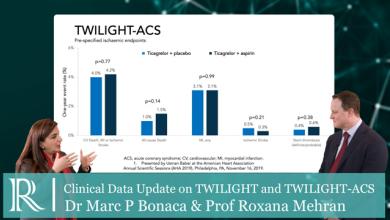
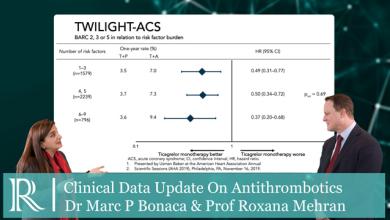
Dual anti-platelet therapy (DAPT) with aspirin and a P2Y12 inhibitor is the current gold standard for the treatment of acute coronary syndrome (ACS). Clopidogrel or ticagrelor are the preferred P2Y12 inhibitor options for initial therapy. Ticagrelor has been demonstrated to have improved efficacy, and is preferred over clopidogrel in the absence of contraindications or the need for oral anticoagulation.
The main risk associated with all antiplatelet therapies is bleeding, and physicians need to carefully weigh the possible adverse effects against the benefits of prescribing these drugs to patients with ACS. Aspirin continues to be prescribed almost ubiquitously for patients with ACS, and P2Y12 antagonists are now often added in; such dual antiplatelet therapy confers greater antithrombotic efficacy but at the risk of increased bleeding. Over recent years, it has become apparent that these drugs may also exert powerful anti-inflammatory effects that provide additional benefit in the management of ACS.